CONTINUOUS RENAL REPLACEMENT THERAPYCRRT
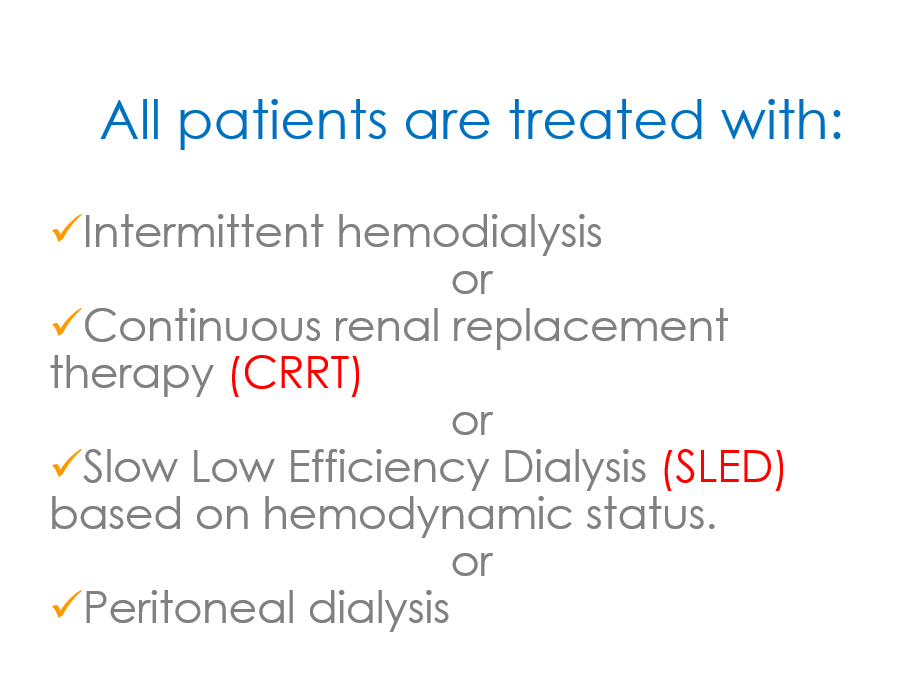
All patients are treated with
Indications of CRRT
Bellomo & Ronco. Critical Care. 2000; 4:339 – 345
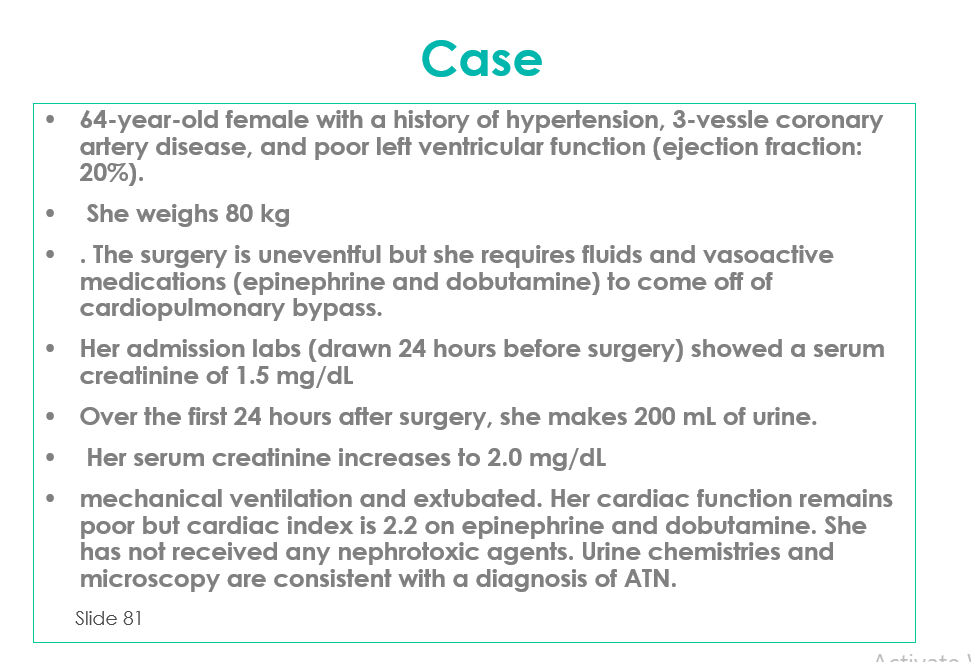
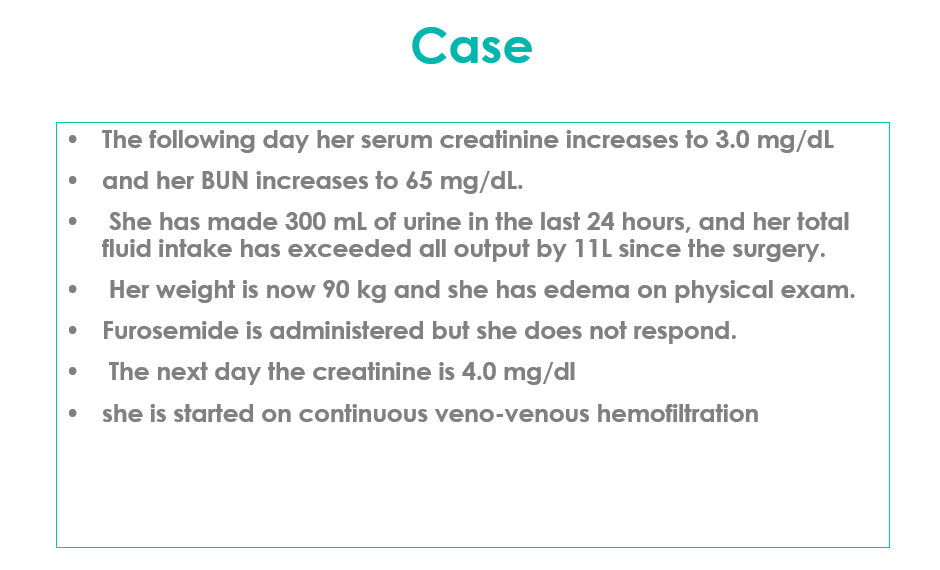
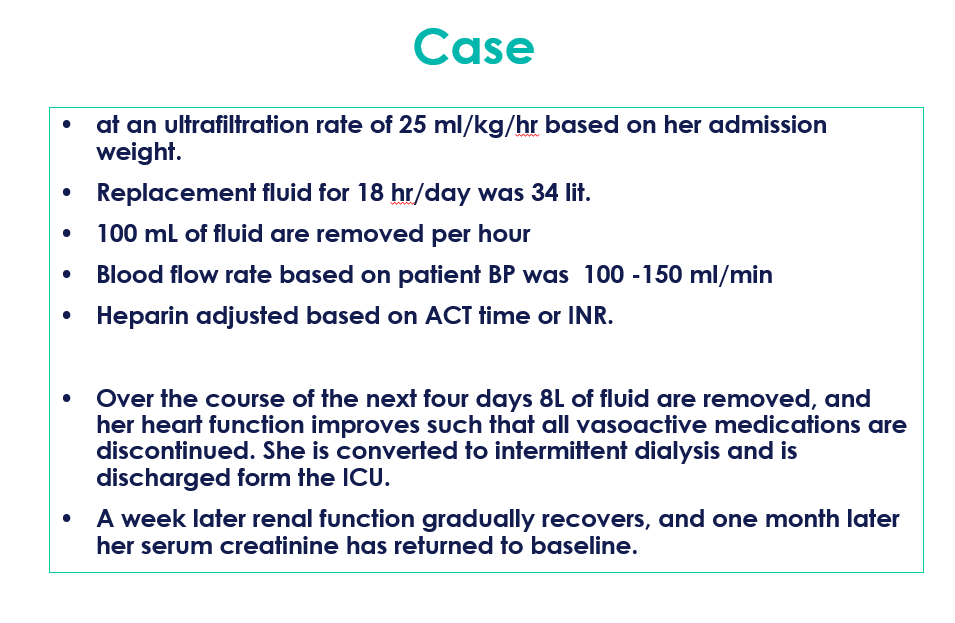
Acute renal failure, which often is a part of multi-organ failure with complications such as shock, cardial and non-cardial pulmonary edema, hemodynamic instability, bleeding, hypercatabolism
Non obstructive oliguria (u/o <200 ml/12 hr) or Anuria.
Severe Acidemia (pH <7.1) d/t metabolic acidosis
sepsis
Hyperkalemia (K >6.5 mmol/L)
Progressive severe dysnatremia (Na >180 or 115 mmol/L)
Suspected uremic organ involvement (pericarditis)
Drug overdose for dialyzable toxins
Hyperthermia (core temp. >39.5oC)
Clinical Conditions to Consider
ARF and need for fluid management related to
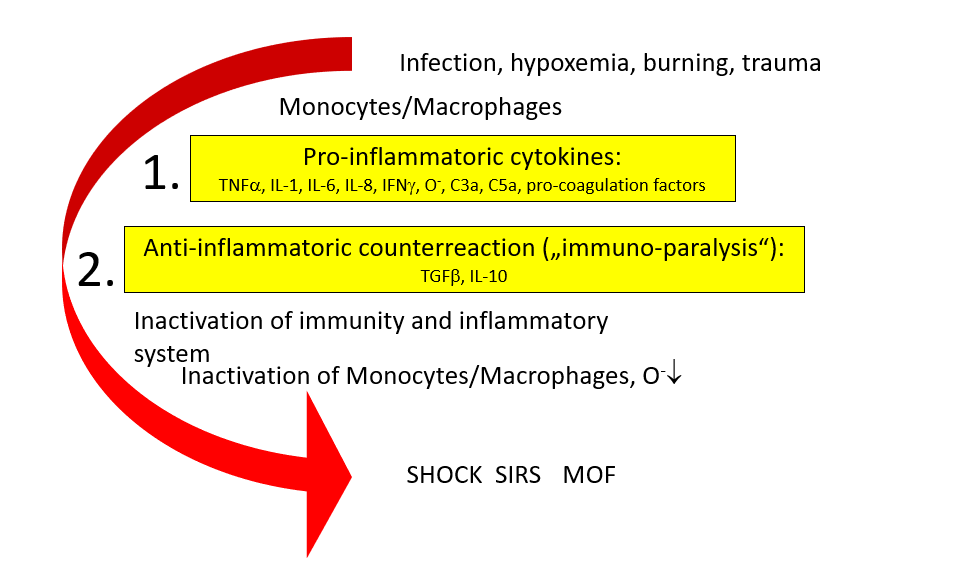
SIRS
Unstable on IHD
Organ transplants
CHF /volume overload
Post CV surgery
Post trauma patients
Severe Burns
What is Sepsis ? ACCP/SCCM Consensus Definitions
(ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. )
Severe Sepsis
Sepsis
Organ dysfunction
Septic shock
Sepsis
Hypotension despite fluid resuscitation
Multiple Organ Dysfunction Syndrome (MODS)
Altered organ function in an acutely ill patient
Homeostasis cannot be maintained without intervention
Infection
Inflammatory response to microorganisms, or
Invasion of normally sterile tissues
Systemic Inflammatory Response Syndrome (SIRS)
Systemic response to a variety of processes
Sepsis
Infection plus
۲ SIRS criteria
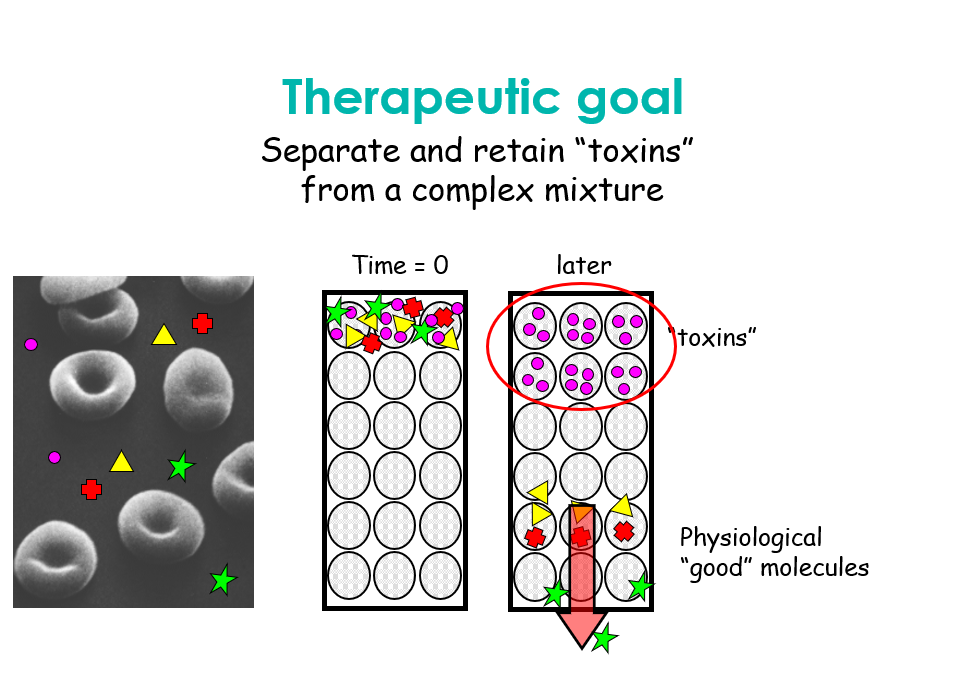
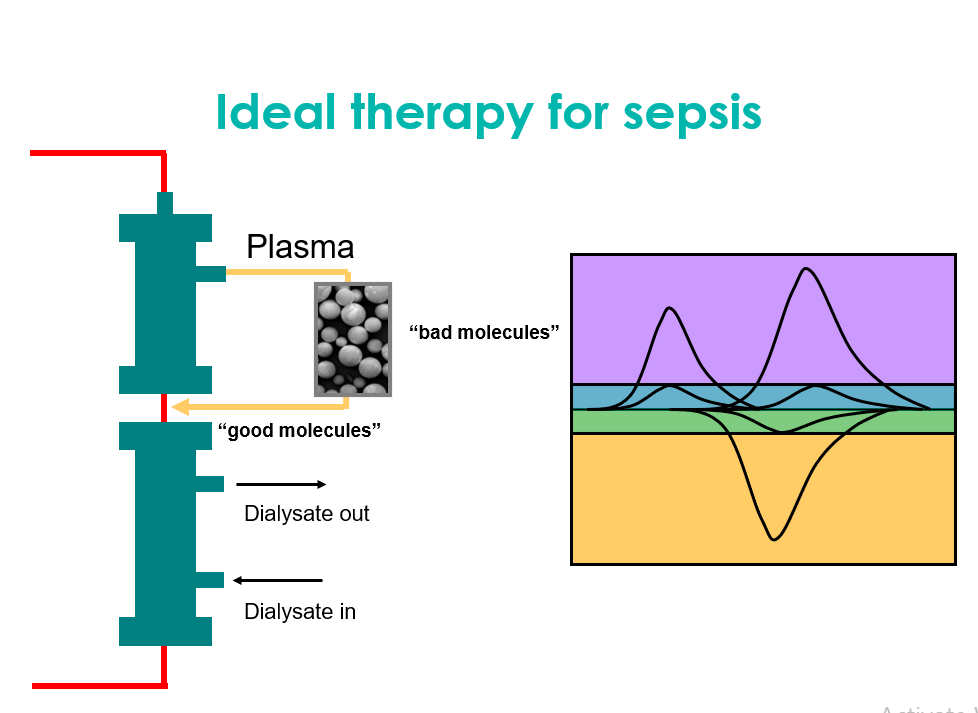
Removal of immunomodulatory substances in sepsis
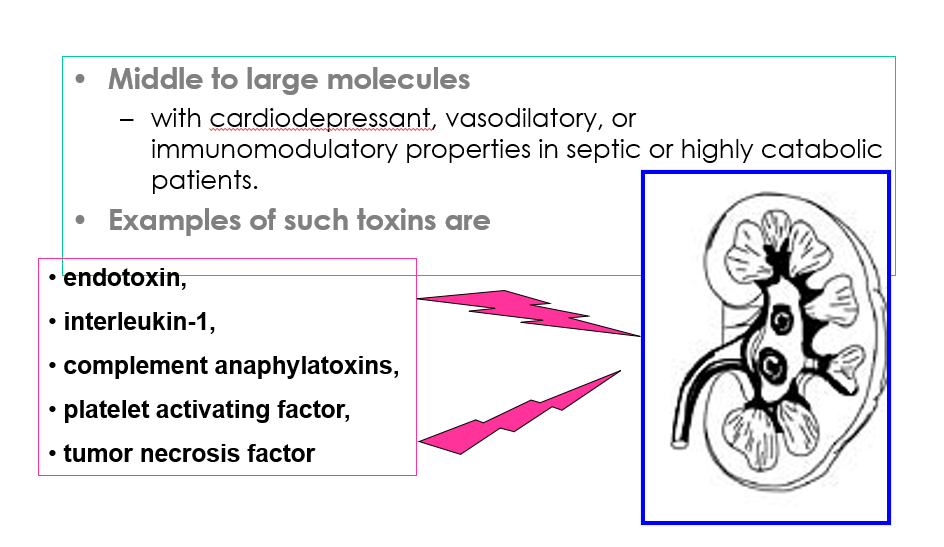
Conclusion
Sepsis & SIRS
The most important complicationof intermittent hemodialysis
۱ – Hypotension % ۲۵ – ۵۰
۲ – Muscle cramp % ۵ – ۲۰
۳ – Arrythmia
Complications
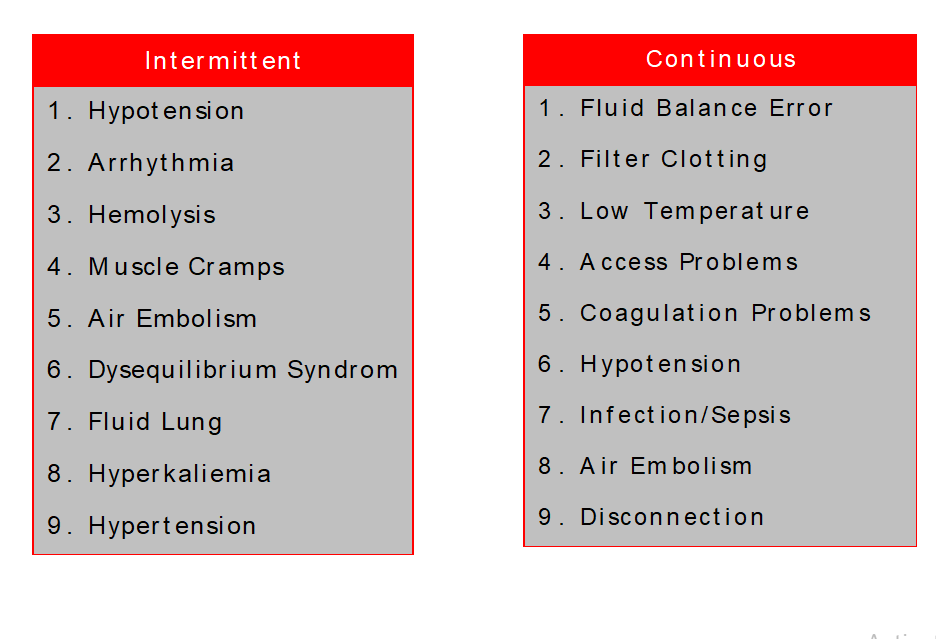
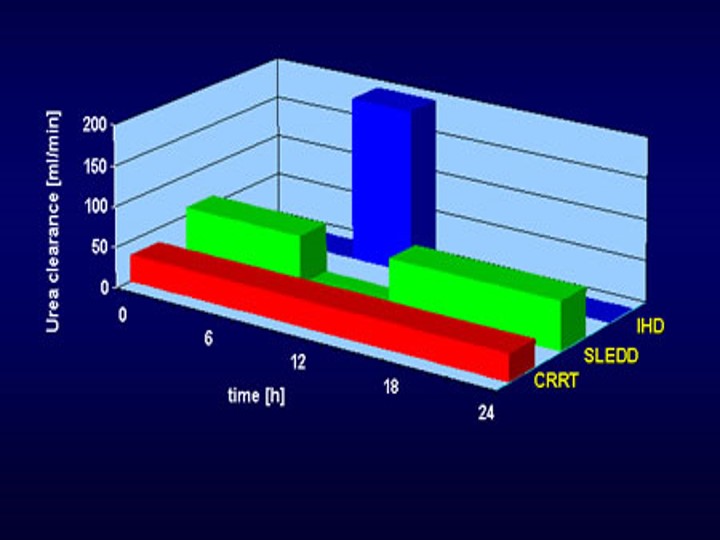
Suitable Dialysis
۱ – Better clinical tolerance
۲ – Better solute clearance
۳ – Improvement acid , base &
electrolytes
۴ – Biocompatibility
۵ – Minimum complications
۶ – Suitable monitoring during the
treatment
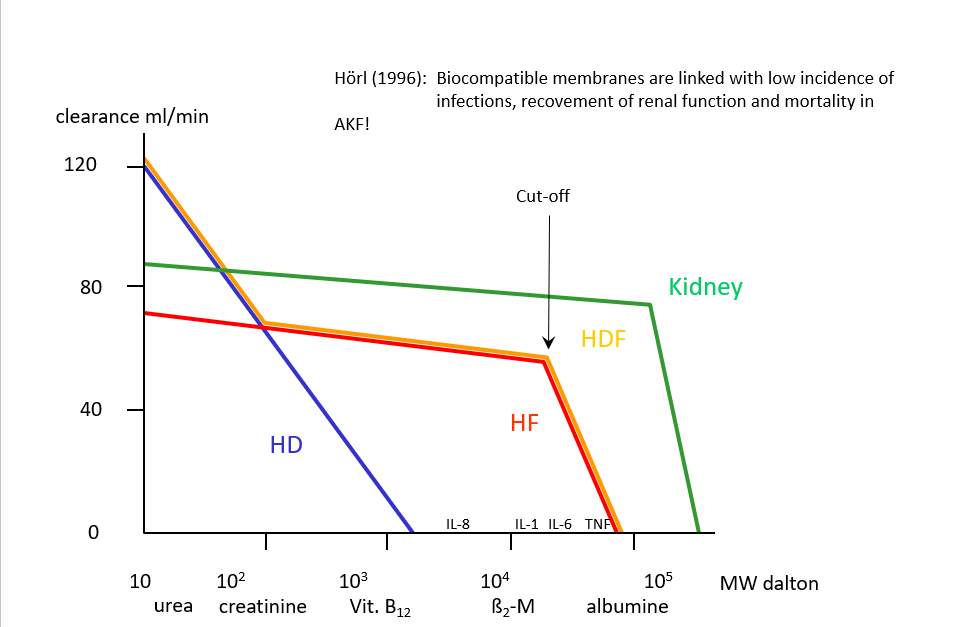
Molecular Weights
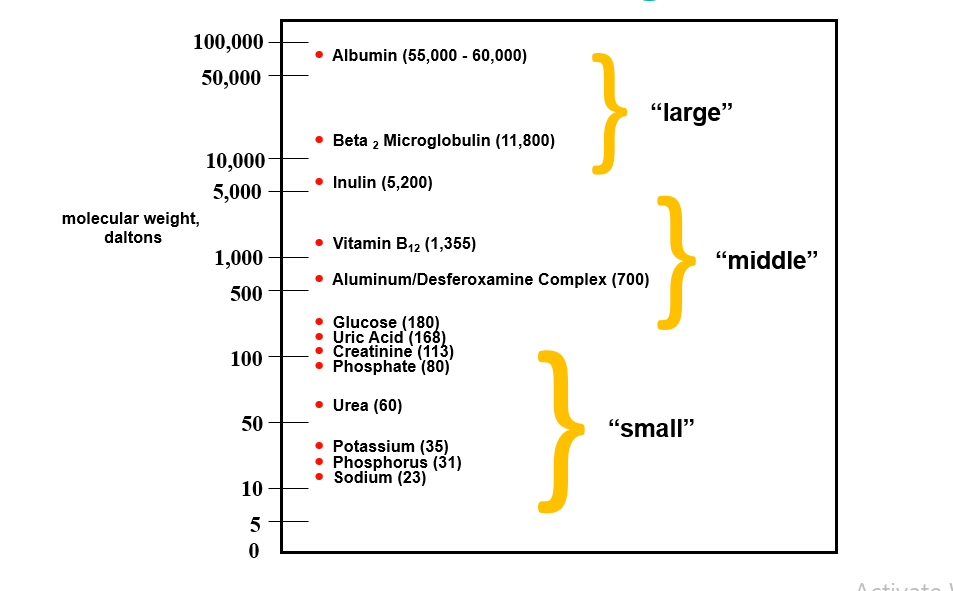
Terminology
Hemodialysis
transport process by which a solute passively diffuses down its concentration gradient from one fluid compartment (either blood or dialysate) into the other
Hemofiltration
use of a hydrostatic pressure gradient to induce the filtration (or convection) of plasma water across the membrane of the hemofilter.
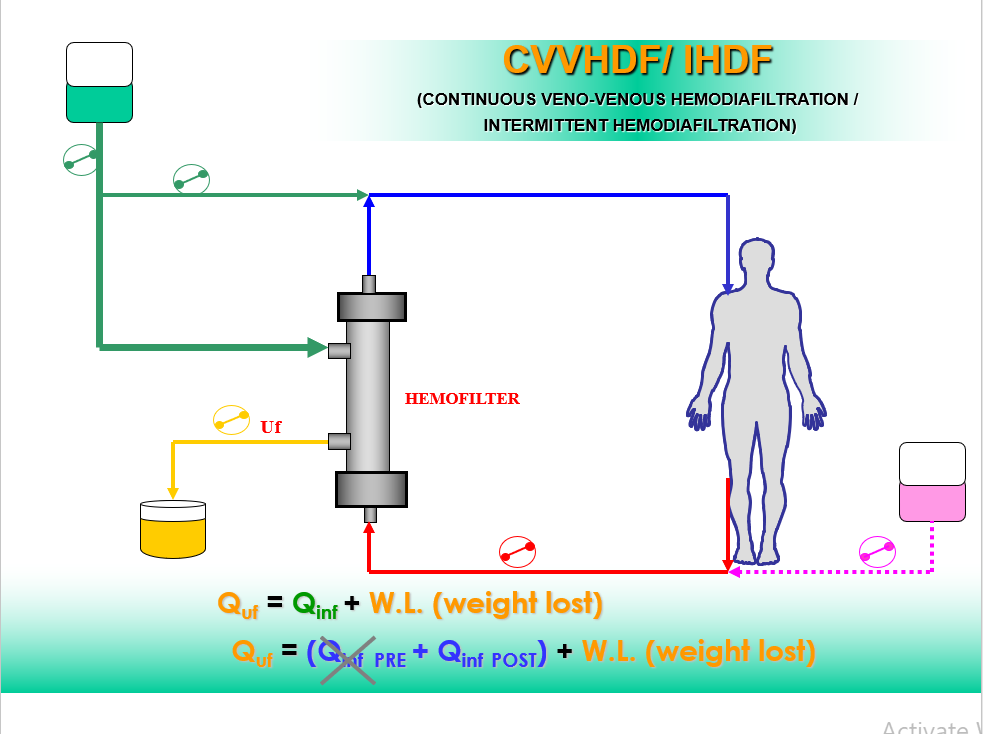
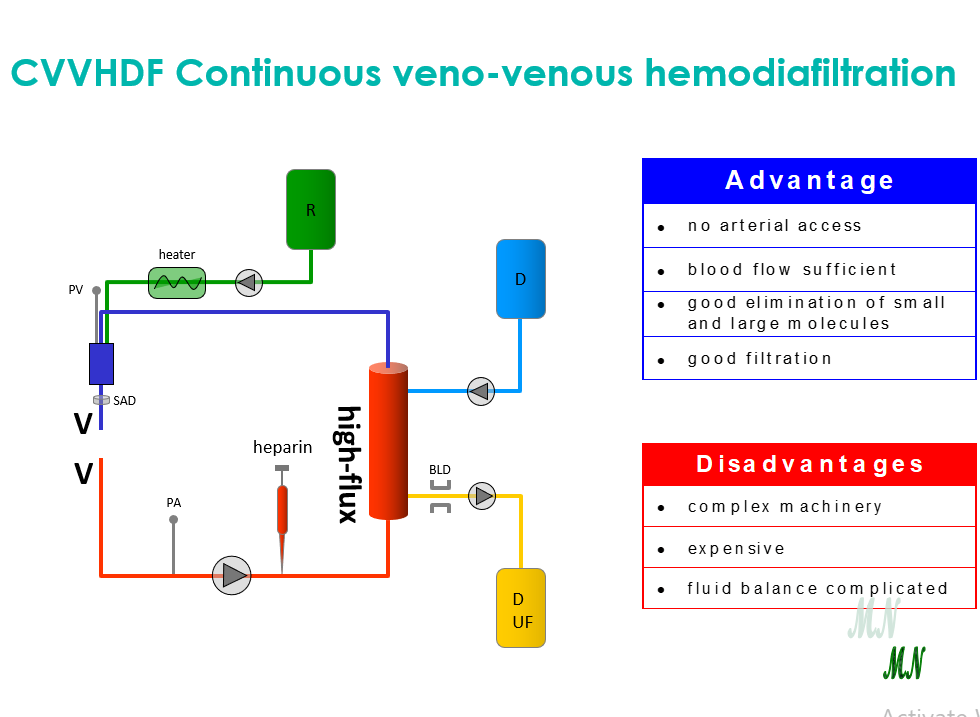
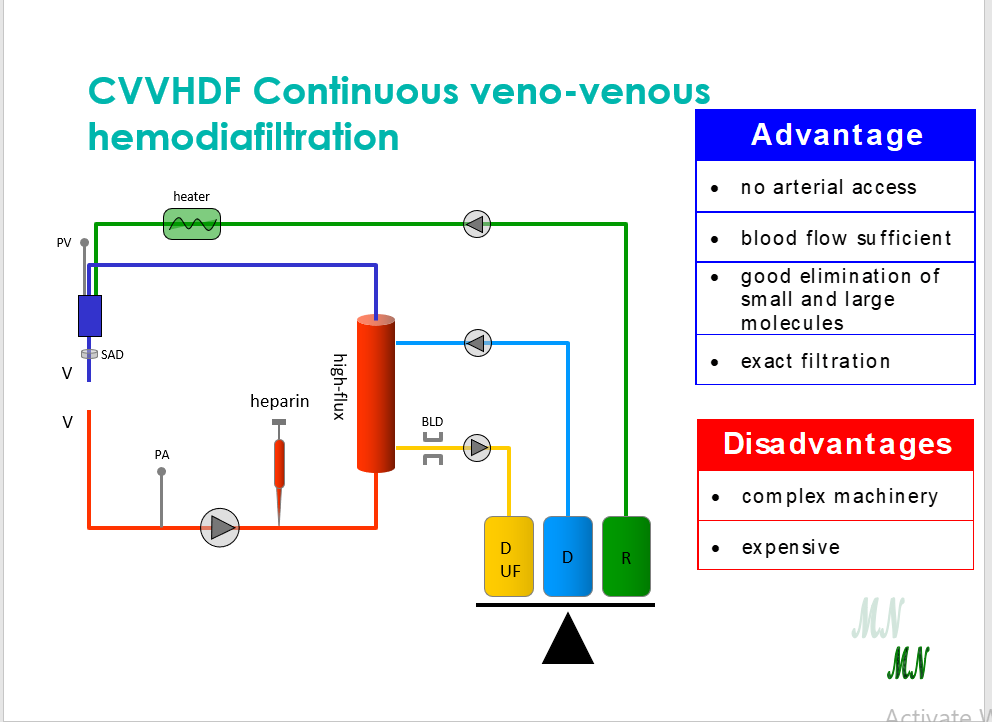
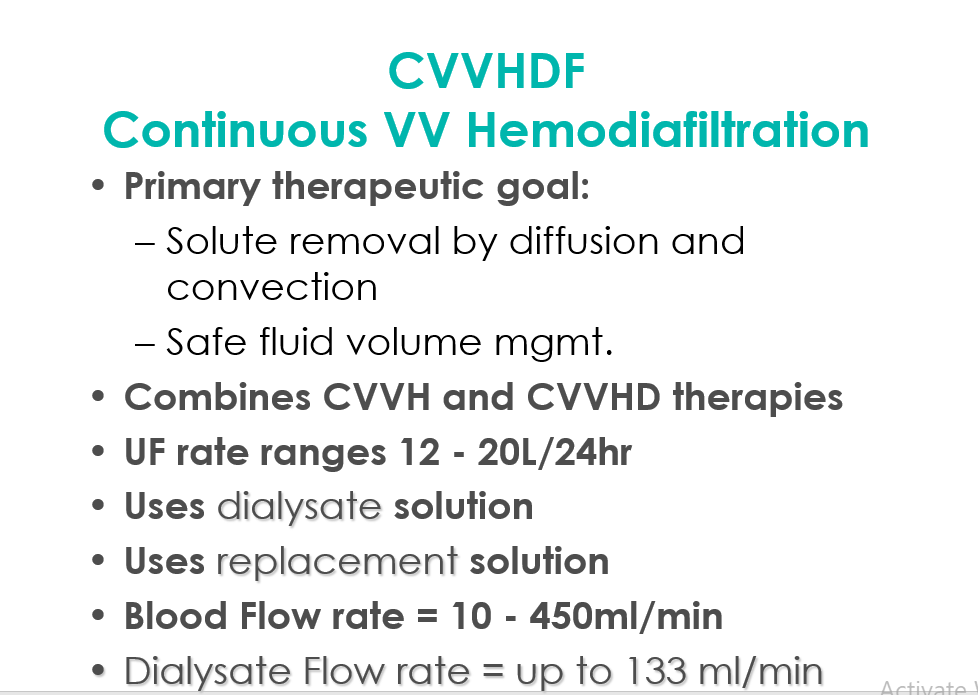
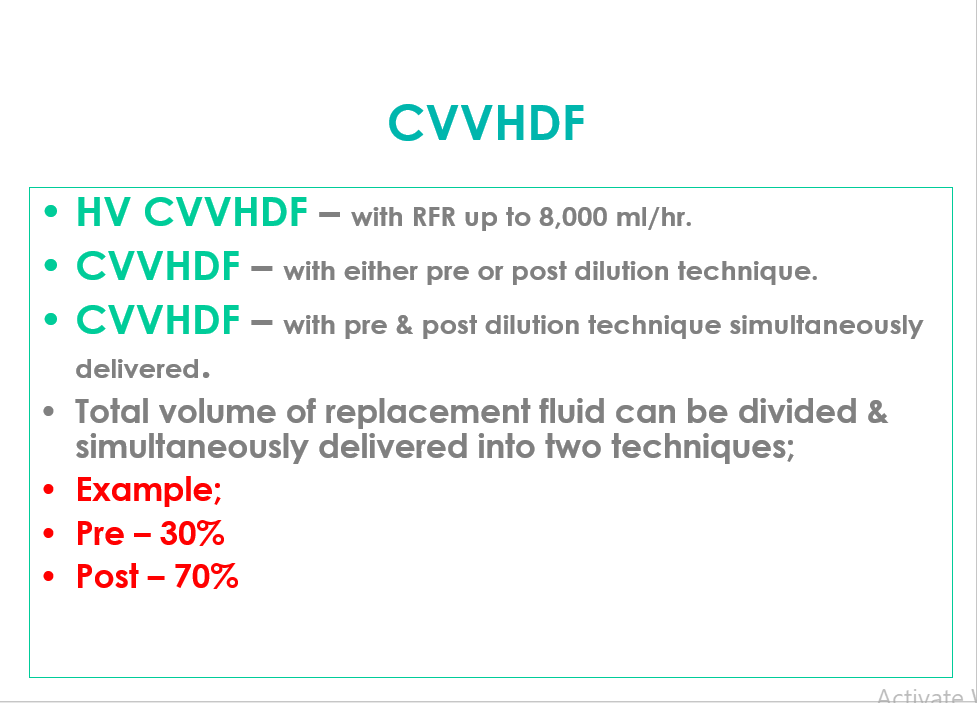
Hemodiafiltration
dialysis + filtration.
Solute loss primarily occurs by diffusion dialysis but 25 percent or more may occur by hemofiltration
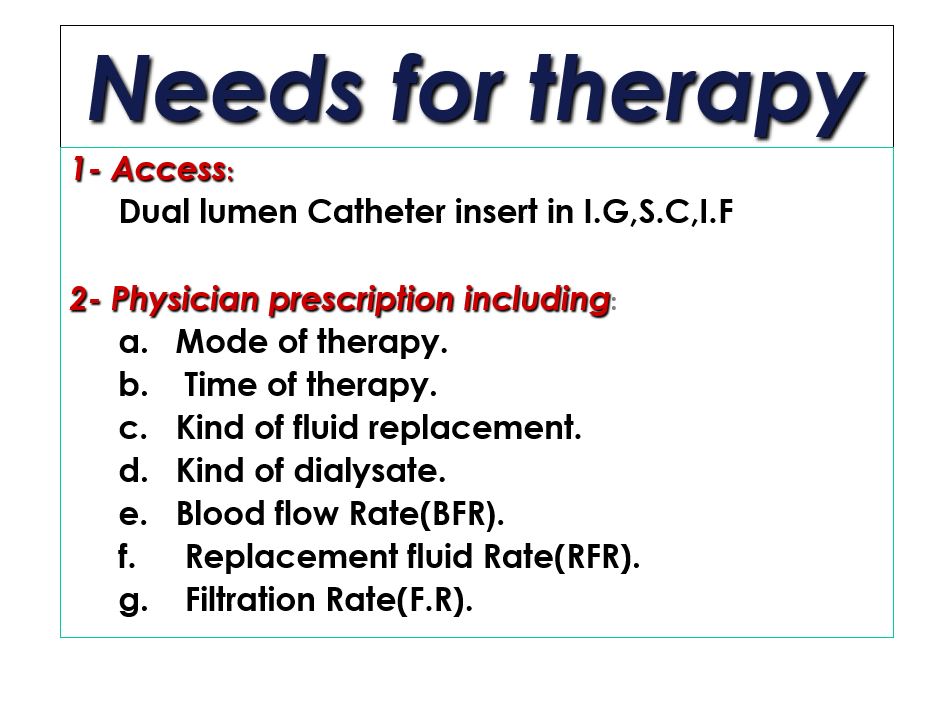
Overview of CRRT
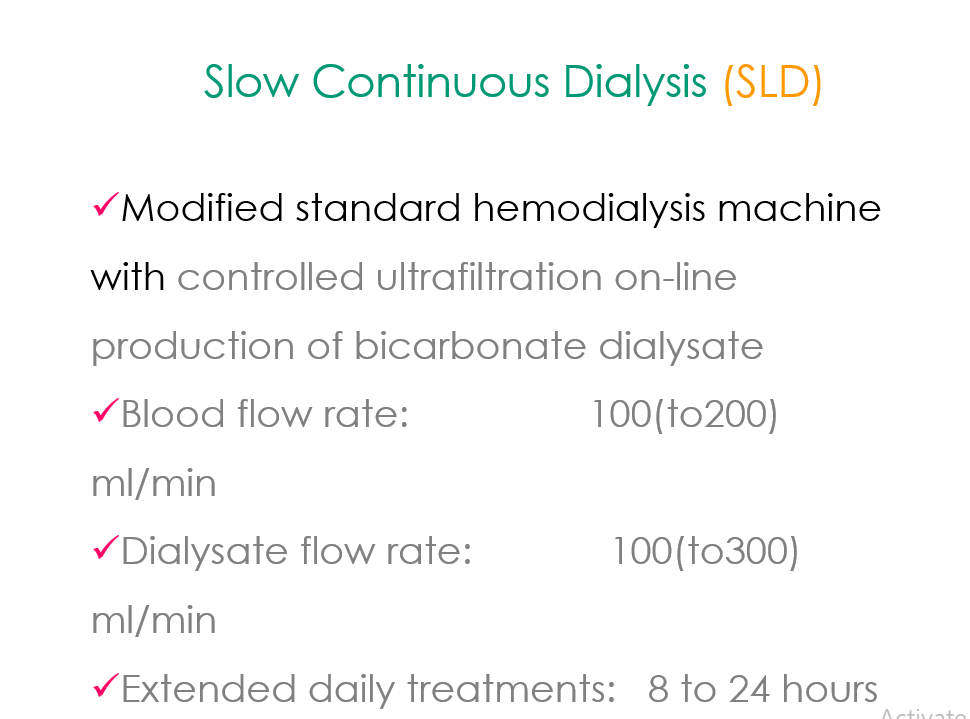
Slow Continuous Therapy
Low Blood Flow Rate
Low Dialysate Flow Rate
Low Replacement Flow Rate
Low Ultrafiltration Rate
THERAPIES
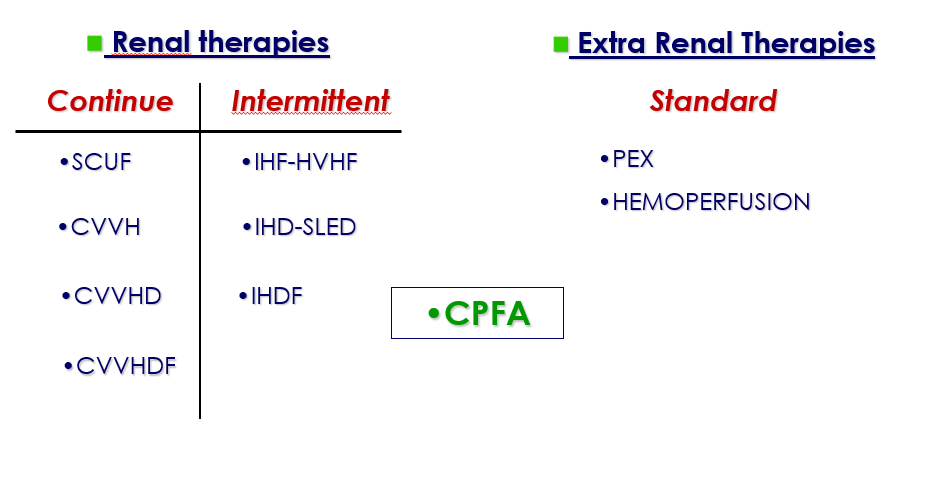
Treatment Modalities
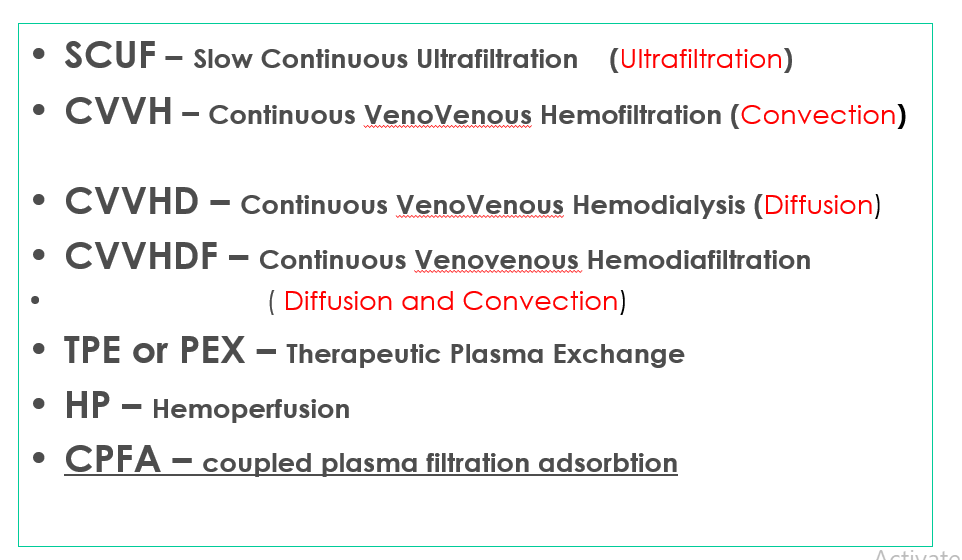
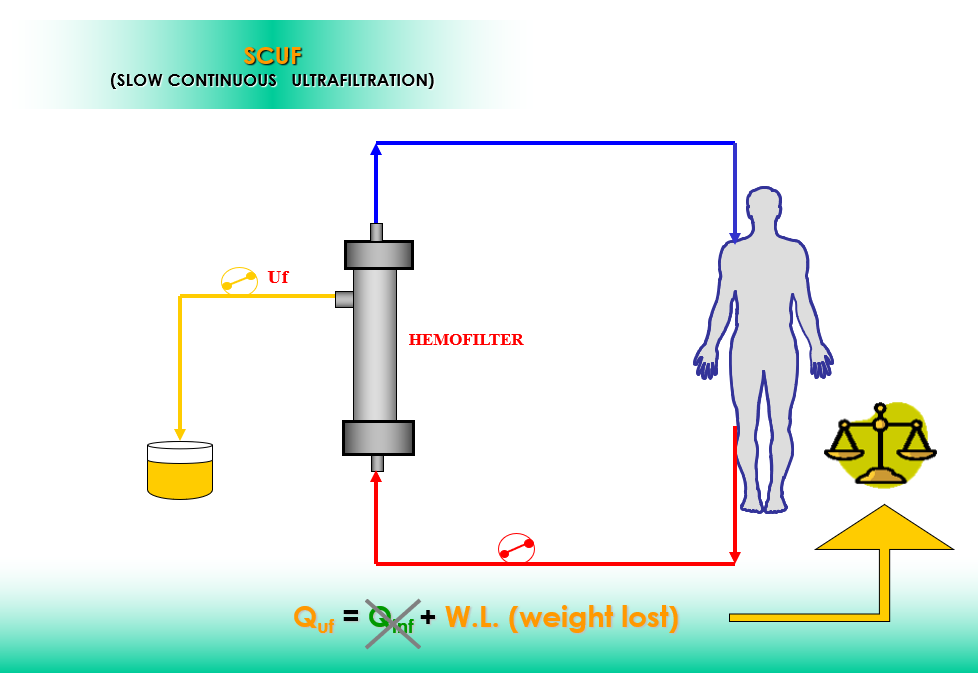
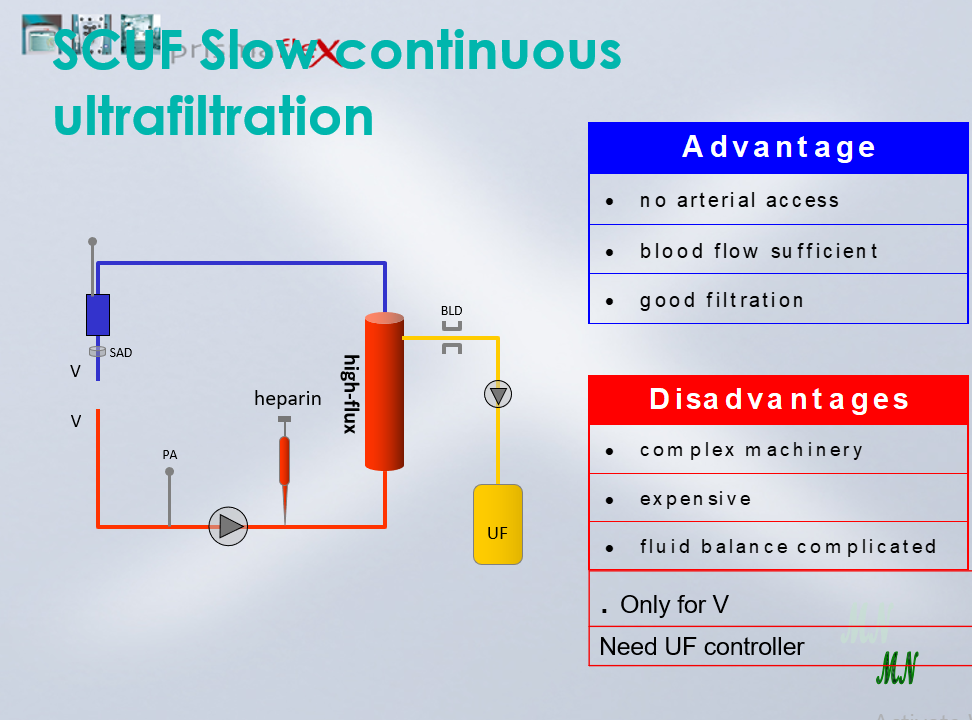
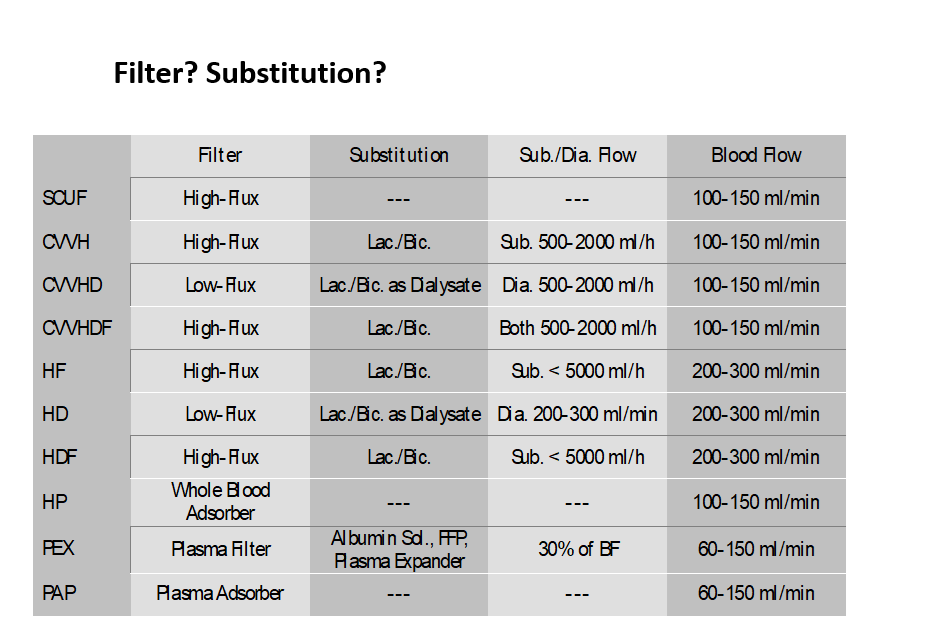
SCUF
Slow Continuous Ultrafiltration
Primary therapeutic goal
Safe management of fluid removal
UF rate ranges up to 2 L/Hr
No dialysate
No replacement fluids
Large fluid removal by ultrafiltration
Blood Flow rates = 10 – 450 ml/min
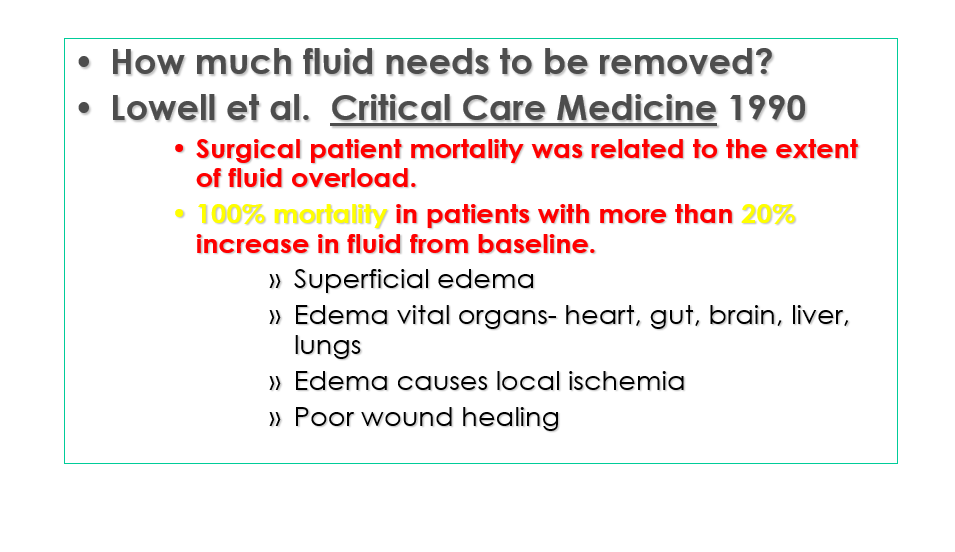
Goals of Fluid Management
Normovolemia
Remove fluid to create a space for fluid therapy (24/7)
Optimize hemodynamic parameters
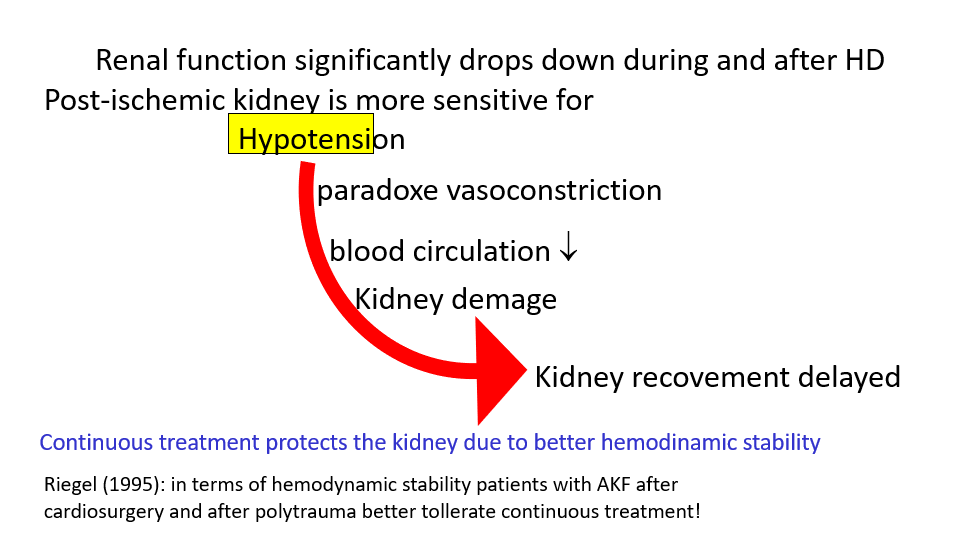
Avoid hypotension – drop down of systemic BP will cause marked fall in renal blood flow and will lead to further damage, insult or injury to kidneys
Fluid Management
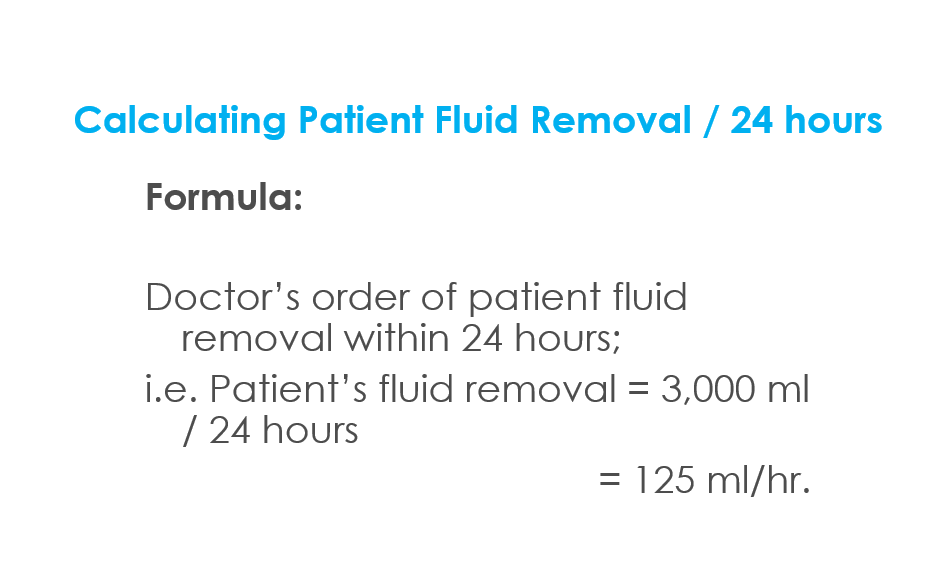
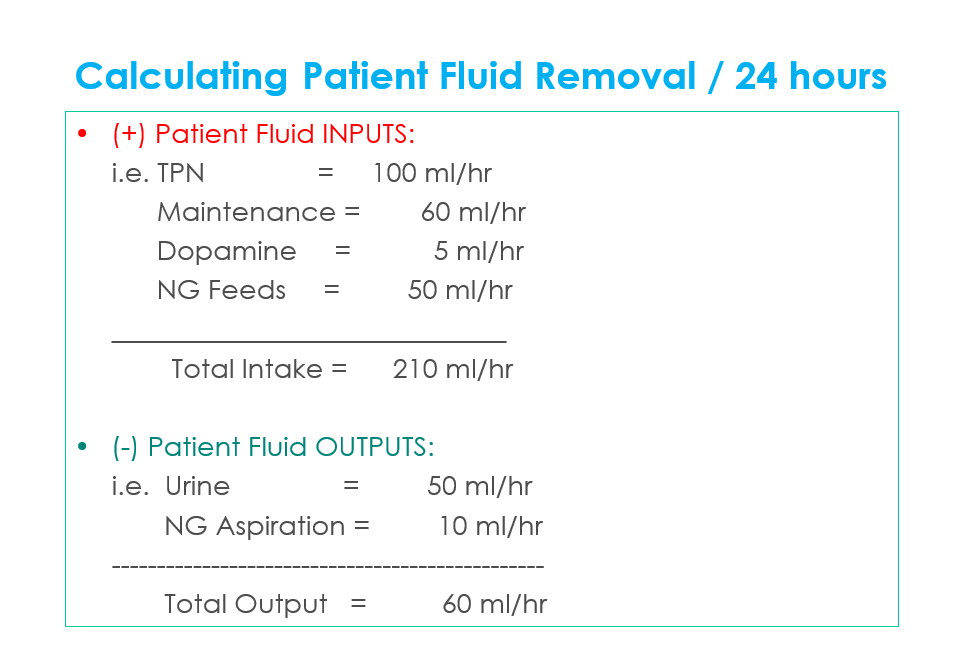
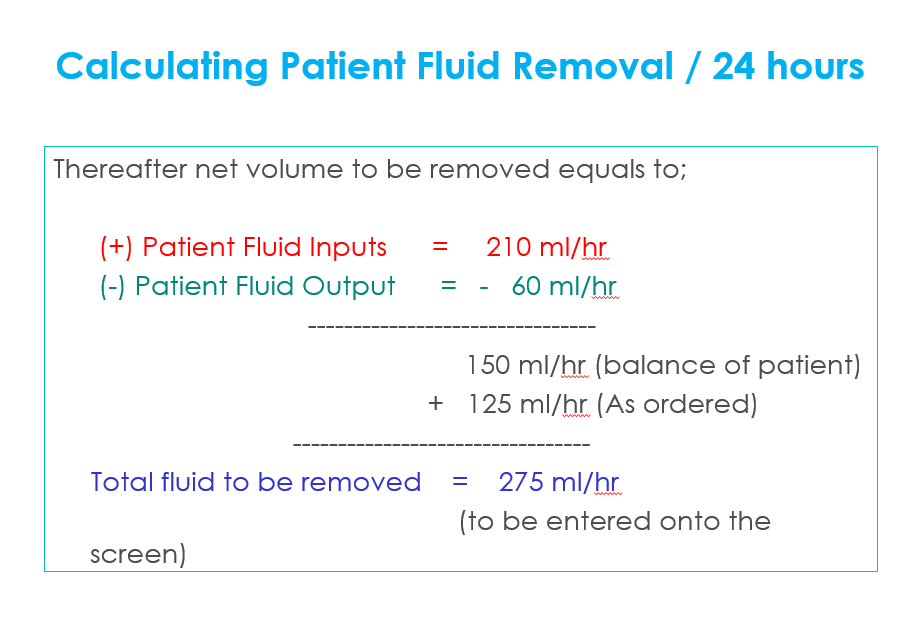
Management
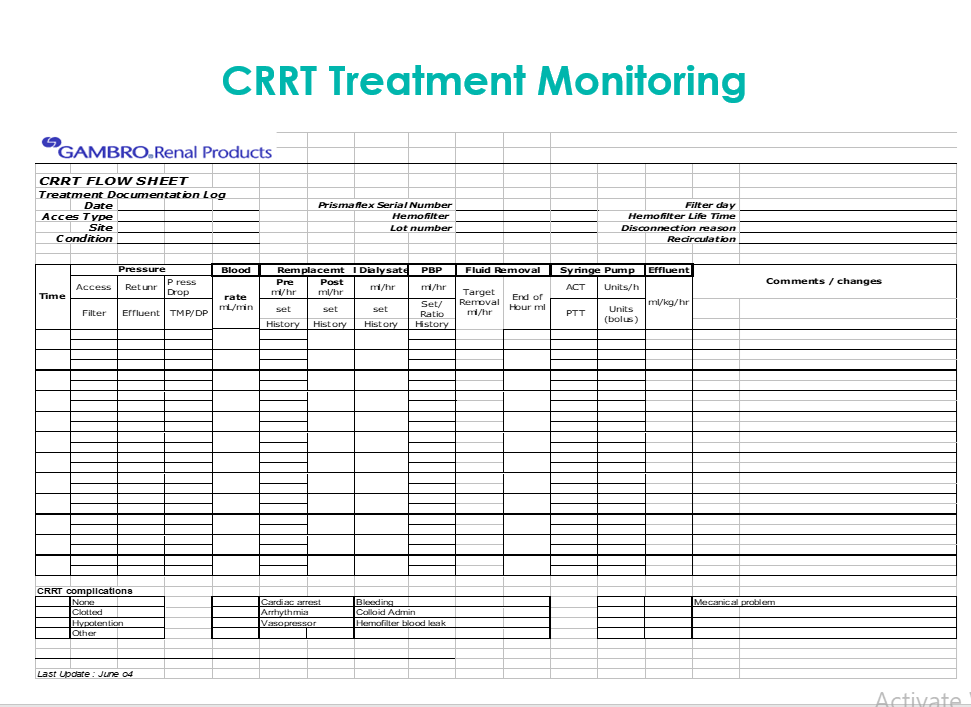
Monitor Intake & Output parameters on the status screen every hour of the machine
Monitor the condition of the patient;
– Excessive fluid loss, will lead to Hypotension and / or Hypovolemia
– Excessive fluid gain, will lead to Hypertension and / or Hypervolemia
END TREATMENT and consult the physician
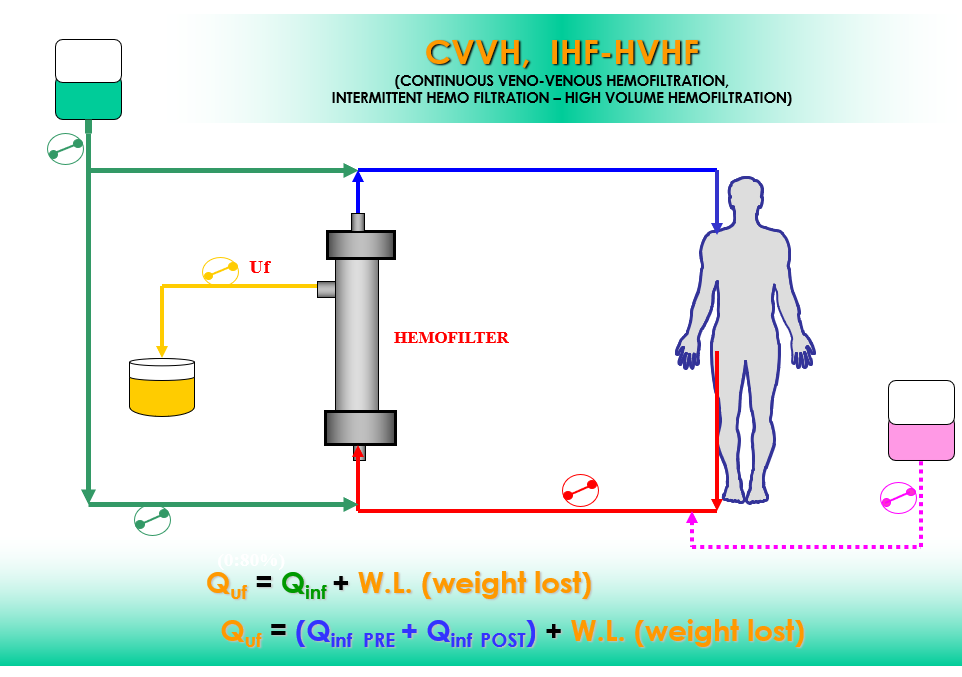
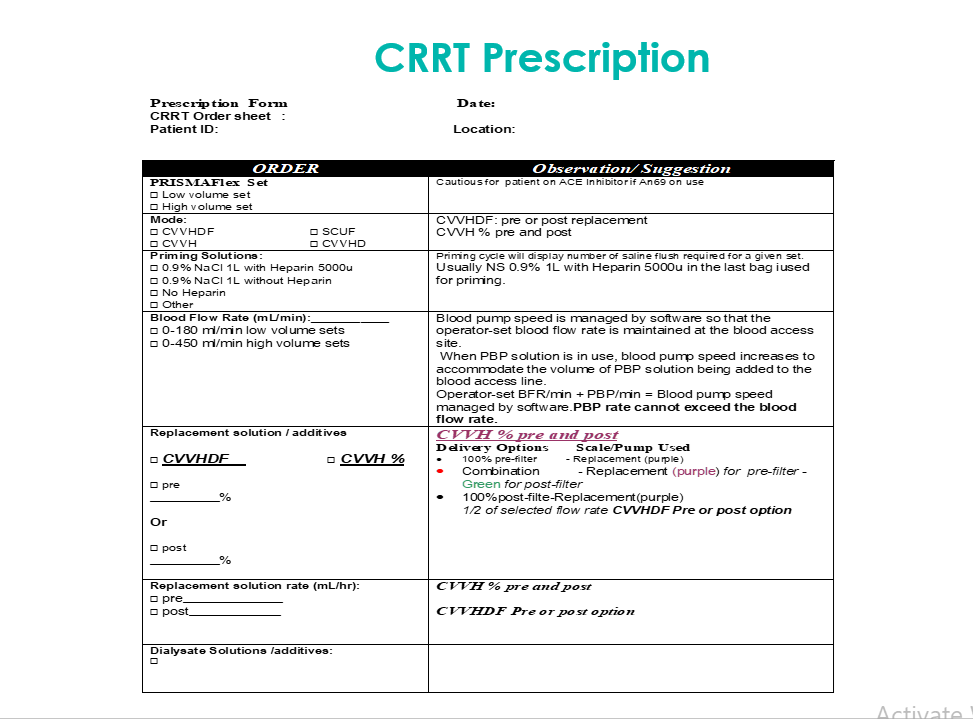
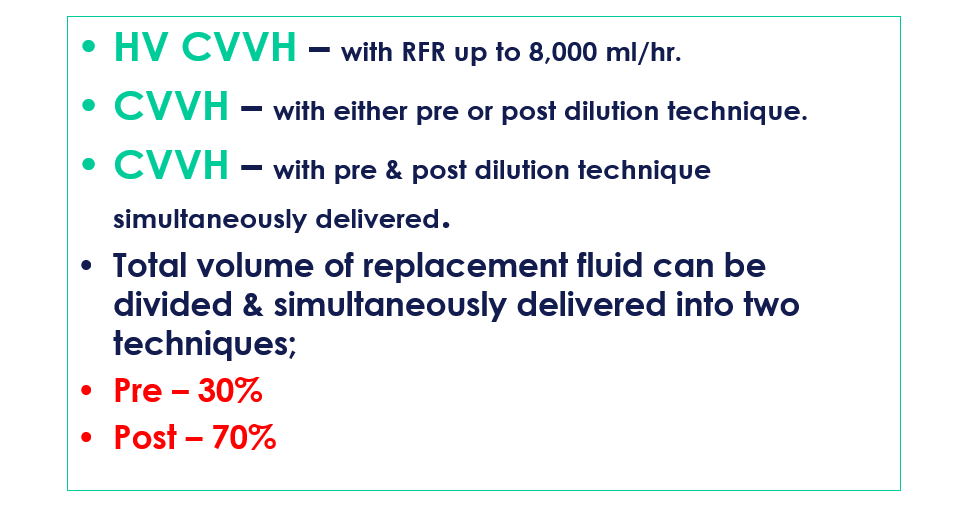
CVVHContinuous VV Hemofiltration
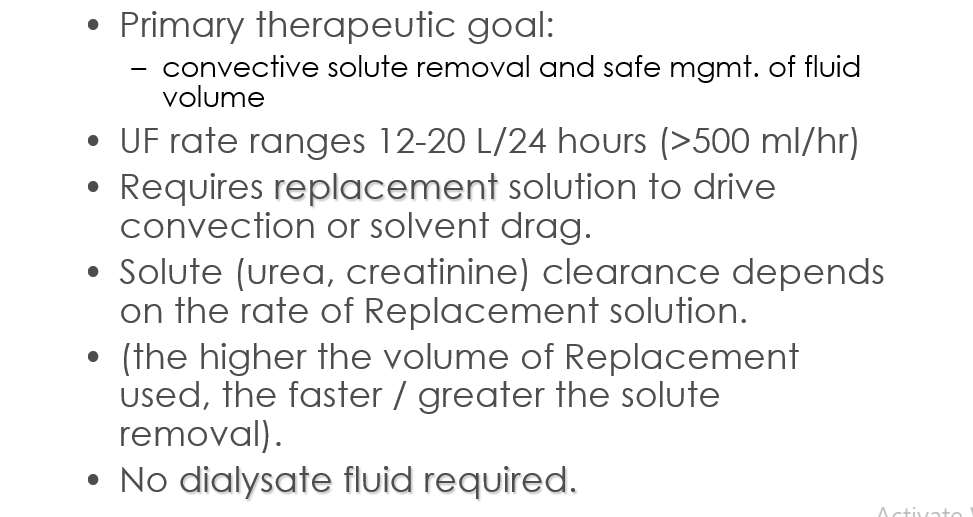
CVVH Continuous veno-venous hemofiltration
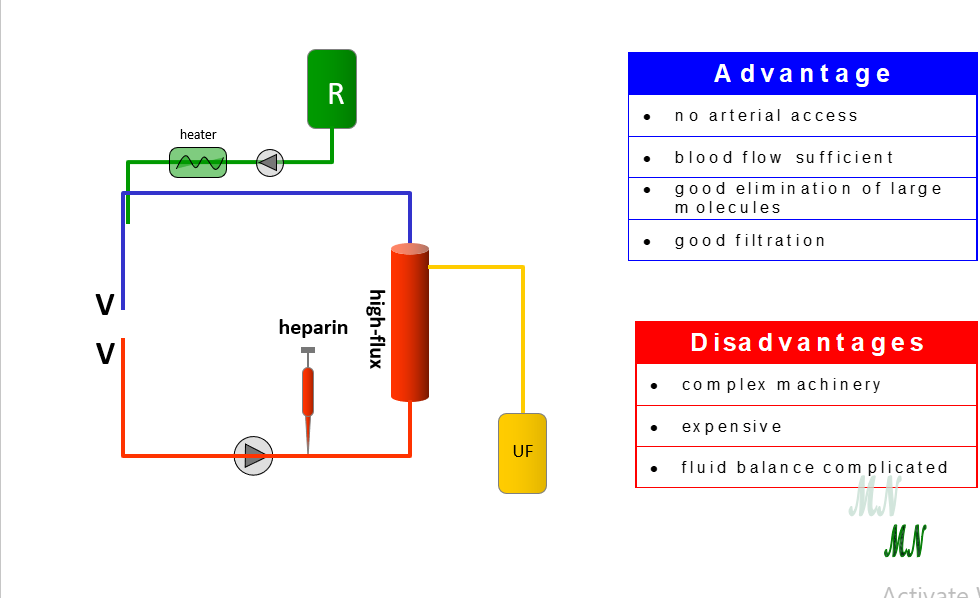
CVVH
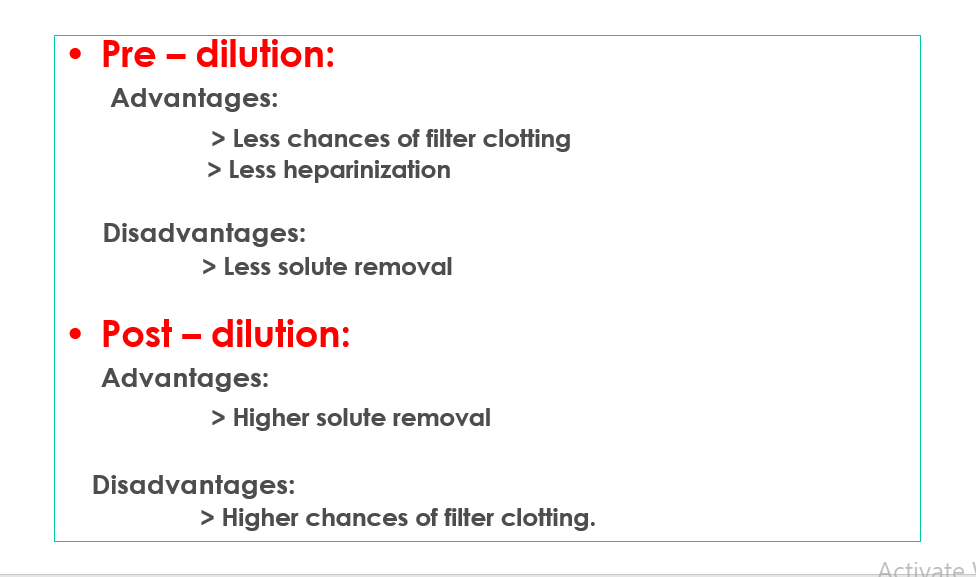
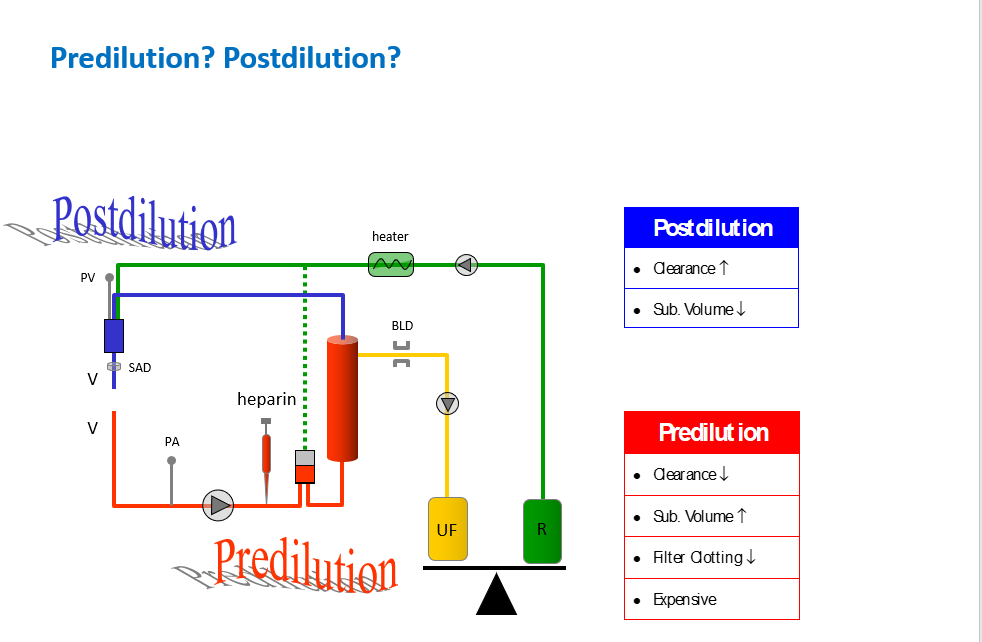
Post filter - dilution
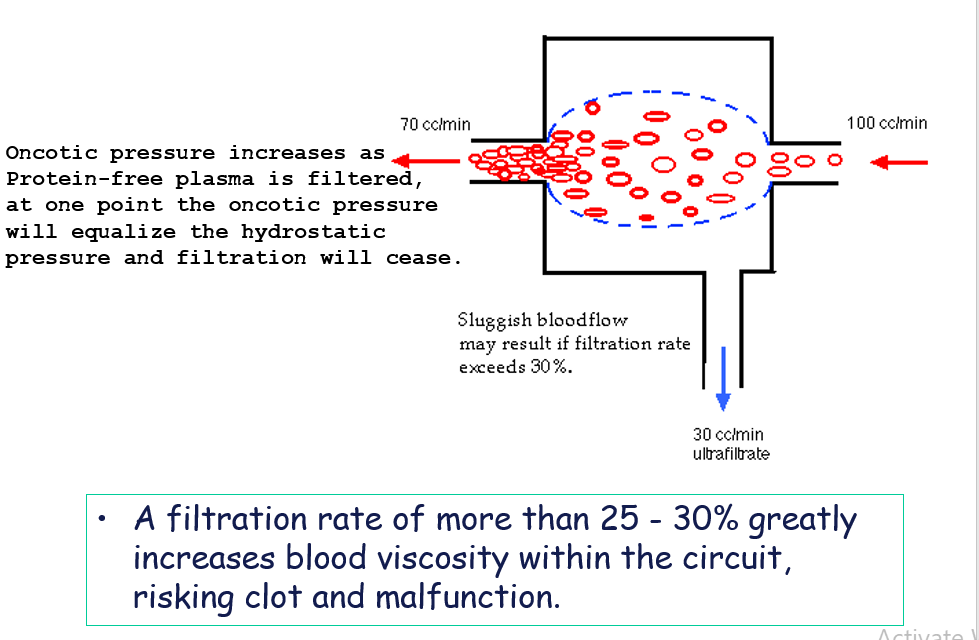
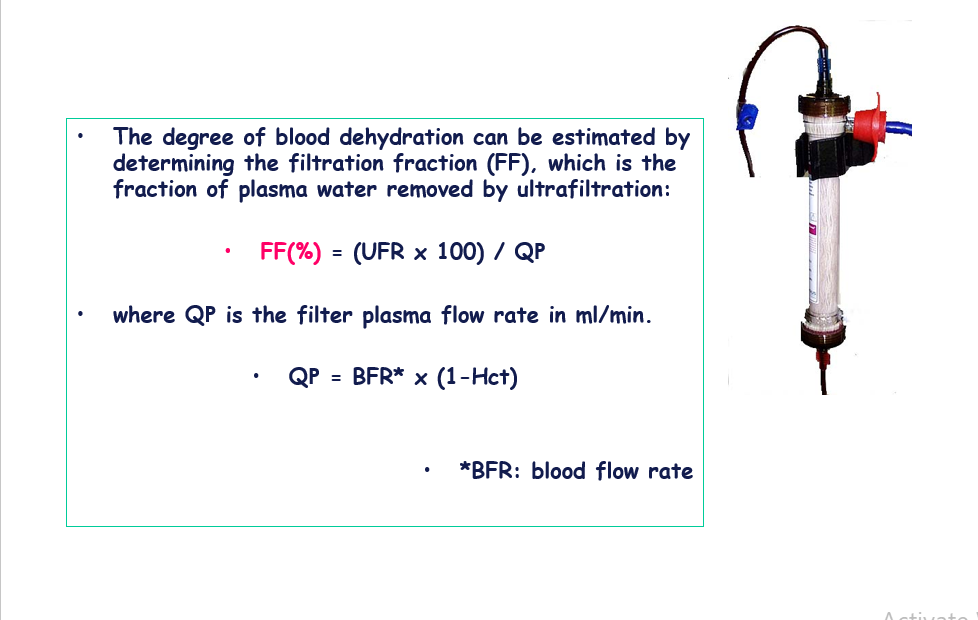
Filtration Fraction
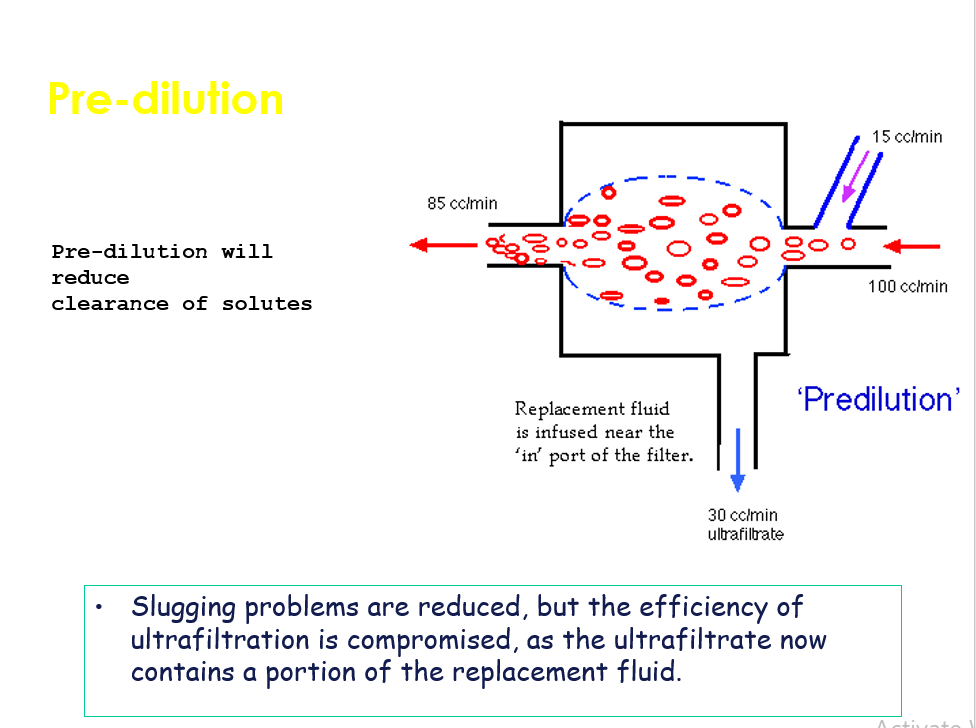
CVVH – Pre dilution
Pre-dilution
CVVH
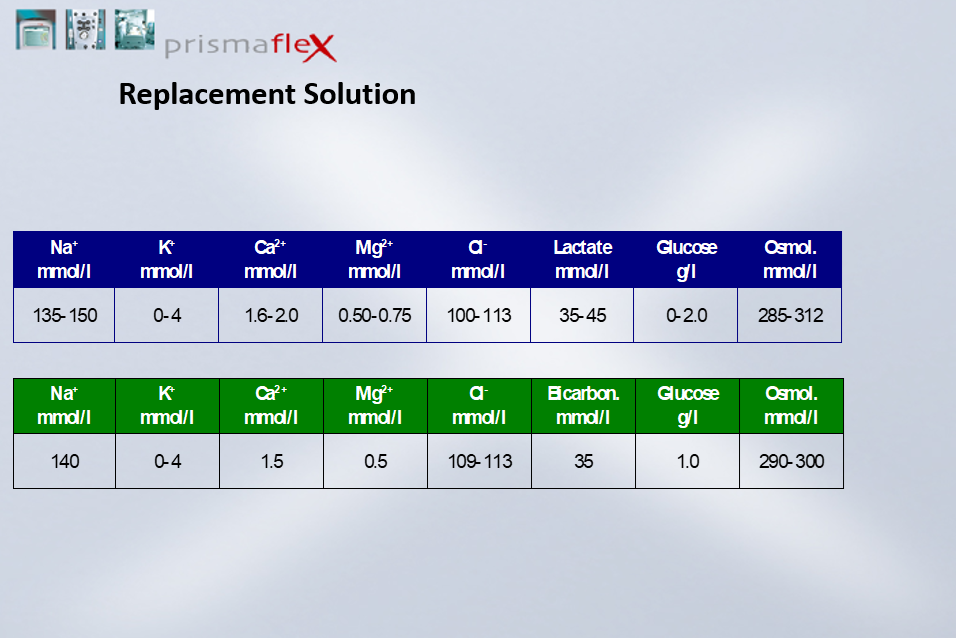
Replacement Fluids
Replacement Fluids
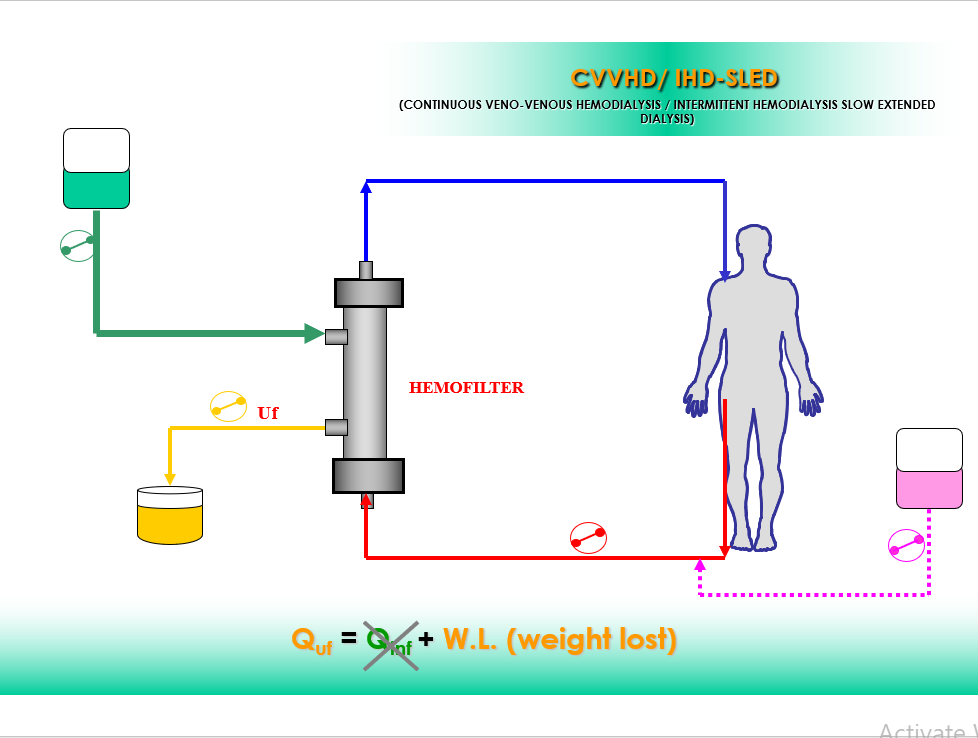
CVVHD Continuous veno-venous hemodialysis
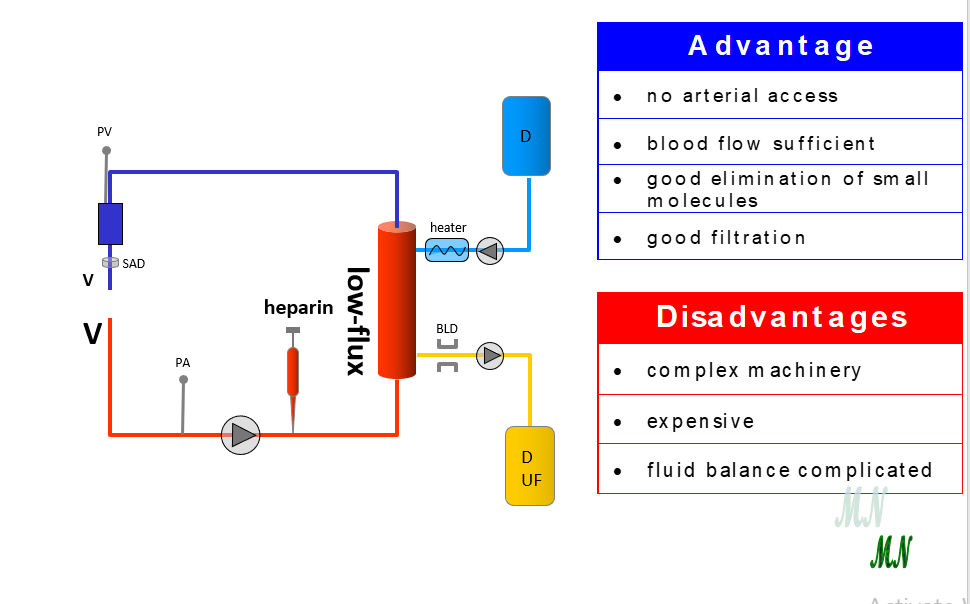
CVVHDContinuous VV Hemodialysis
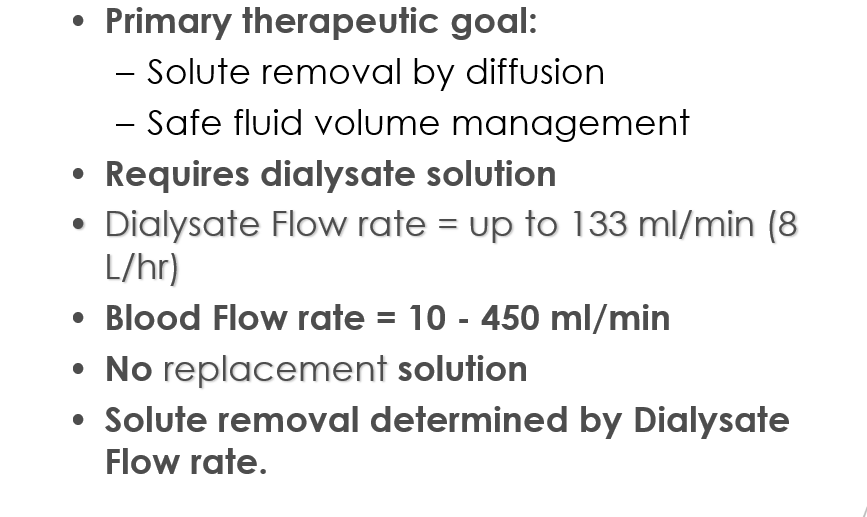
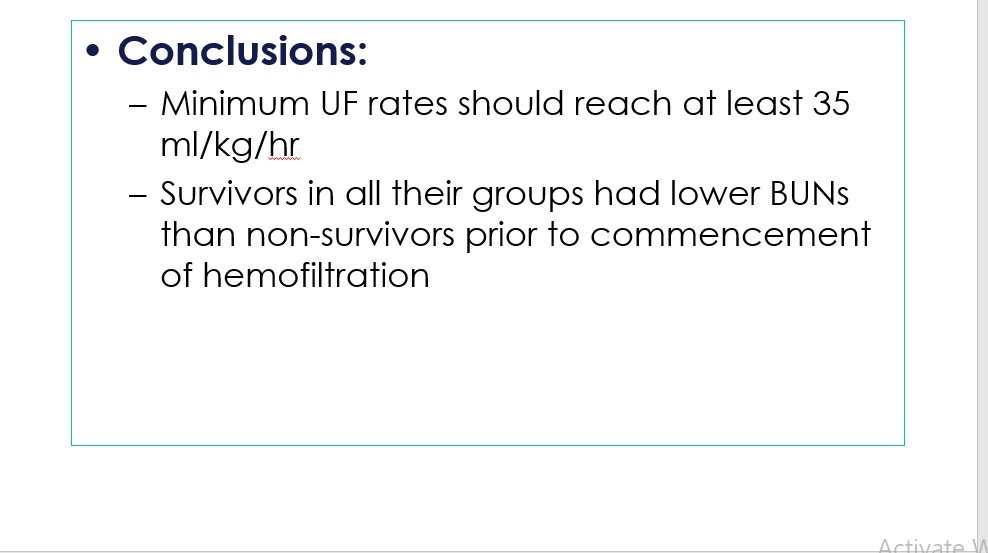
Ronco et al. Lancet 2000; 351: 26-30
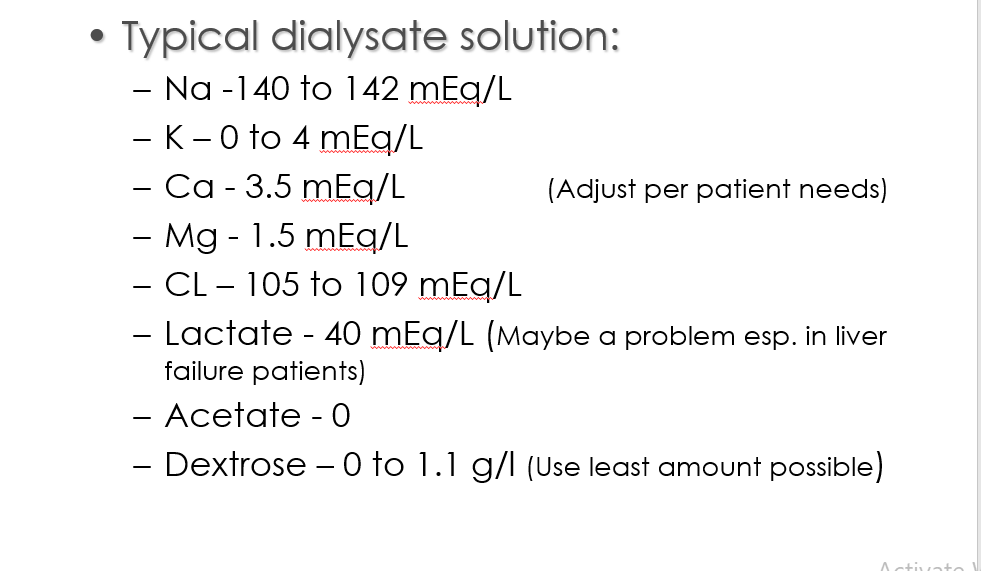
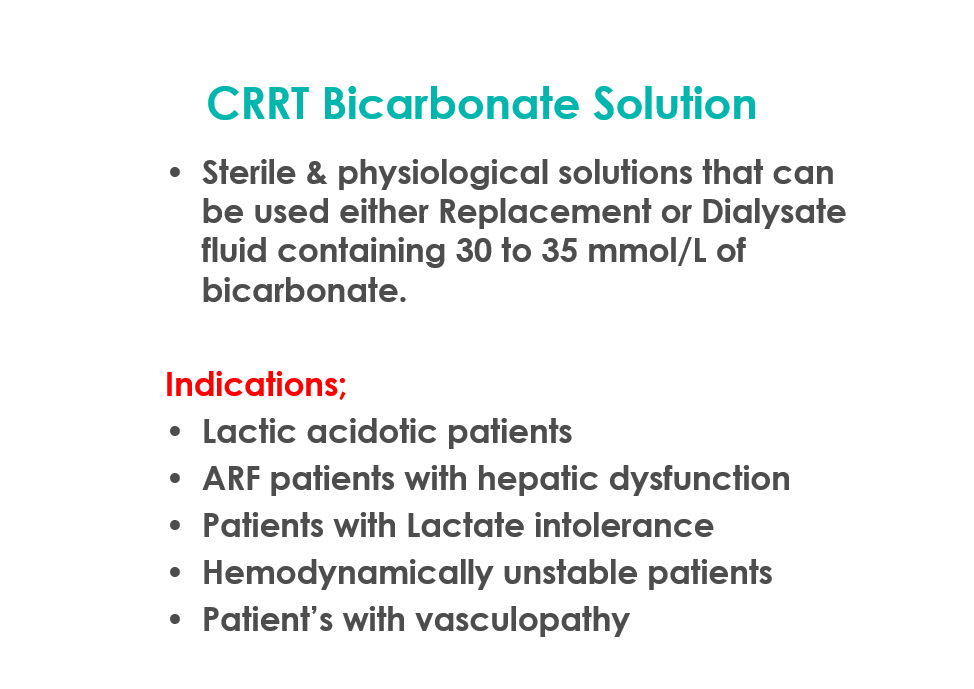
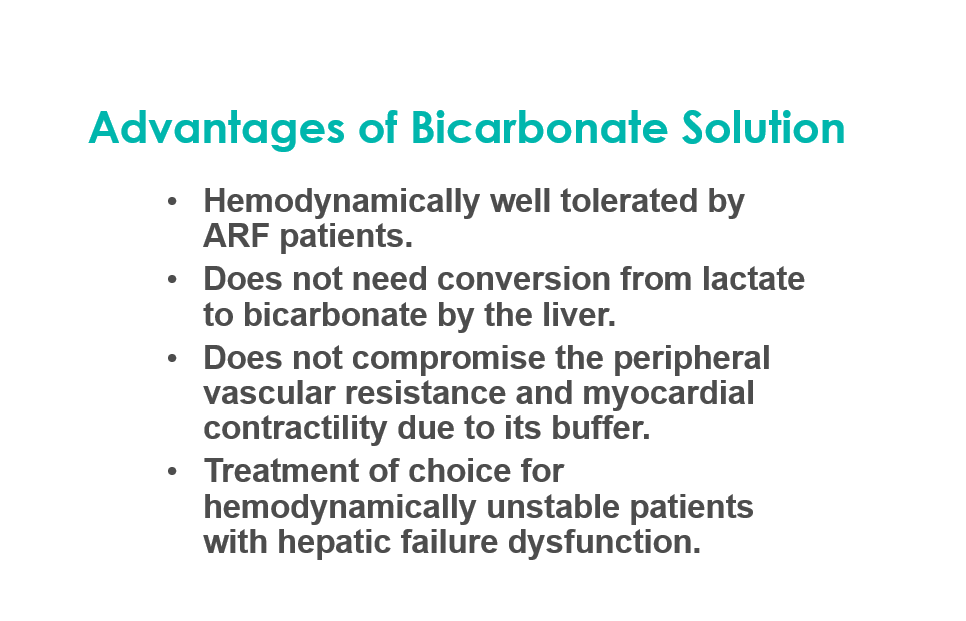
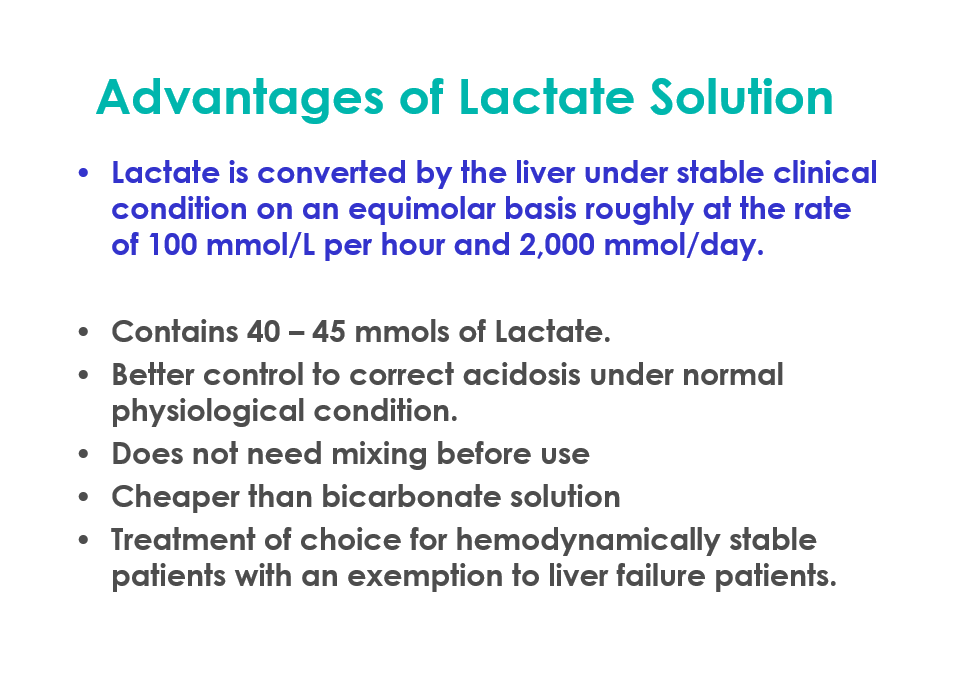
Dialysate Solutions
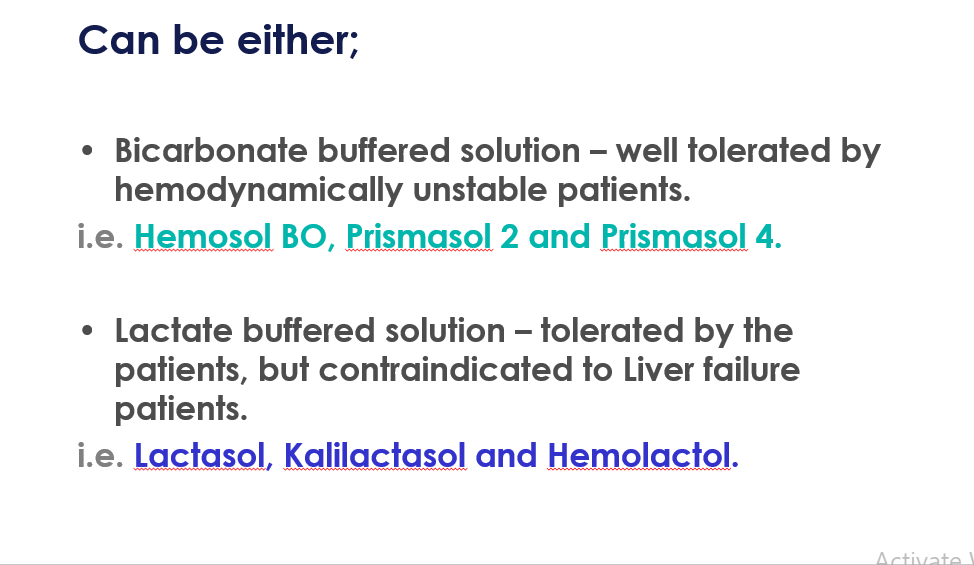
Dialysate Solutions